 I am a big proponent of standardization. In fact, I often call it “my one-string banjo”. When I made the move from the aerospace industry to healthcare, I was appalled at the lack of standardization and resistance to it. I have been quoted as saying, “there are 7 CRNA’s performing the process 9 different ways”, because not even one person does it the same from one time to the next!
I am a big proponent of standardization. In fact, I often call it “my one-string banjo”. When I made the move from the aerospace industry to healthcare, I was appalled at the lack of standardization and resistance to it. I have been quoted as saying, “there are 7 CRNA’s performing the process 9 different ways”, because not even one person does it the same from one time to the next!
There are many opportunities for standardization in healthcare. But that does not mean “cookbook medicine”. I would never think, even for a minute, that I can (or want) to dictate how a physician treats a disease, or how a surgeon performs an operation. They are highly-trained, caring experts, who try to make the best use of the evidence they have to cure their patients. Every patient is different, because every human body is different. Therefore, physicians should be allowed, even encouraged to always make the best decision for the patient right in front of them, not for “the majority” of patients.
The opportunities for standardization in healthcare that I focus on and I encourage my teams to focus on are in the processes that happen before or after that physician is treating that patient, and in the systems that support those processes. There is so much waste (transportation, inventory, motion, waiting, over-processing, over-production and defects – “TIM WOOD”) in these processes that they account for 30%, or even more, of the total healthcare expenditures in the United States, or about $1 Trillion!
Standardization can help eliminate some of this waste by honing in on the variability and mistakes that generally plague most of these processes.
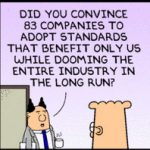
NEVERTHELESS, standardizing just for the sake of standardizing is just as bad as resisting it! In a recent Value Stream Map exercise looking at opportunities to reduce waste for cataracts surgery, a team was questioning why they performed a certain step during room turnover between two cases of cataracts surgery. That step in particular did not make sense for cataracts surgeries. As we (I was facilitating the VSM exercise) kept prodding into this issue, it finally came out that “about five years ago, they said, ‘we are standardizing everything, so you will do this step for all surgeries’, regardless of the type of surgery”. I cringed, took a deep breath, and allowed the team to continue down their continuous pursuit of perfection. They proposed to eliminate that step and, after a few short weeks, the change was approved and that is now the “new standard”. Eliminating that step saves between six to eight minutes of turnover time, which can amount to more than two extra cases per day of surgery!
When I heard the explanation about why they performed this step, it was as if somebody took the name of “standardization” in vain! I love standardization, I preach it every day, but I also always say that Lean concepts are not earth-shattering; they are based on common sense. So, when somebody intentionally adds a step that adds no value to a process in the name of standardization, I take offense!
This is not standardization. This is perhaps laziness for not wanting to spend the time understanding the process and assess what adds value and what does not. It is a lack of common sense or, at the very minimum, it is ignorance of the core concepts of value and waste. It is a lack of respect for the people performing these processes and it is NOT Lean!
Therefore, I say to you, standardization is a beautiful thing. It is never about telling a physician how to treat a patient or how to perform a surgery. It is never about blindly doing a set of steps with complete disregard of whether they add value or not. It is about documenting and communicating the best, fastest, safest way we have of performing a process today, so we can improve upon it tomorrow.
Have you heard or seen the name of standardization taken in vain?

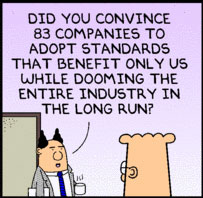
I’d like to get your opinion in standardizing processes in educating our healthcare workers within our 10 hospital healthcare system.
Taking into account that AHA has guidelines on how to teach their courses that offers 2 options of content delivery (instructor-led and blended learning), we implemented a policy that, as a training center, we will only teach the courses using the blended learning model.
Blended learning model meant that students must take an online exam in conjunction with an instructor led skills session.
We opted for this type of curriculum because of several identified problems including lack of instructors, staff underperforming in skills and exams, non-compliance with reading materials prior to an instructor led classes, and the length of an instructor-led courses.
Representatives from each facility met and decided as a group (albeit having 1 or 2 that was not entirely on-board) that blended leaening will help us with all our current issues. Policy regarding this was finalized and approved by all chief nursing officers in each facility.
Fast-forward six months, I received complaints from one of the instructors that one facility was non-compliant and is still delivering instructor led training WITHOUT the mandatory online coursework.
I wasnt sure how I feel about this since another reason why I suggested this option to the group is because of the poor quality of the instructor led course in the same facility prior to the policy implementation.
This example is just one of the many when dealing with “standardization” in our health care system. I felt that we have done our part to identify issues, planned and implemented a process that promotes quality patient care but was largely ignored due to resistance in moving forward to the digital world.
Do you think I have used the word “standardization” in vain in this situation? What could we have done better? How can I make them understand our intent? This facility did not even give the process a chance to be evaluated.
Standardization does not mean “black or white” as everything has some sort of gray area but we even gave them the flexibility of choosing several of the other variables in the process. The only thing we asked to be consistent is the implementation of the online course as a requirement for completion.